Tāpiri Mai, a project co-designed with the community to improve access to healthcare for whānau on Matakana and Mōtītī Islands in the Bay of Plenty, has entered a new phase focused on building health literacy. Following three years of work to strengthen infrastructure, systems for telehealth and expand access to services, locally delivered diabetes self-management sessions marked the start of a new chapter.
Project Manager Moira Lomas says the shift reflects community aspirations. “Our focus now is helping whānau feel capable in managing their own health needs. They want to make informed decisions and take charge of their wellbeing.”
To plan this phase, the team reviewed local health data. Diabetes stood out as a clear priority. On Matakana Island, 24% of patients are diabetic or pre-diabetic, which is 2.4 times the rate across the wider Western Bay of Plenty Primary Health Organisation (WBOP PHO).
Whānau had been invited to WBOP PHO diabetes self-management groups on the mainland, but limited barge times made attendance difficult. The solution was simple: take the sessions to the island. Thirteen people attended the two Matakana sessions in November 2025, and seven joined remotely from Mōtītī using the Wi-Fi infrastructure installed for telehealth.
Designed with purpose
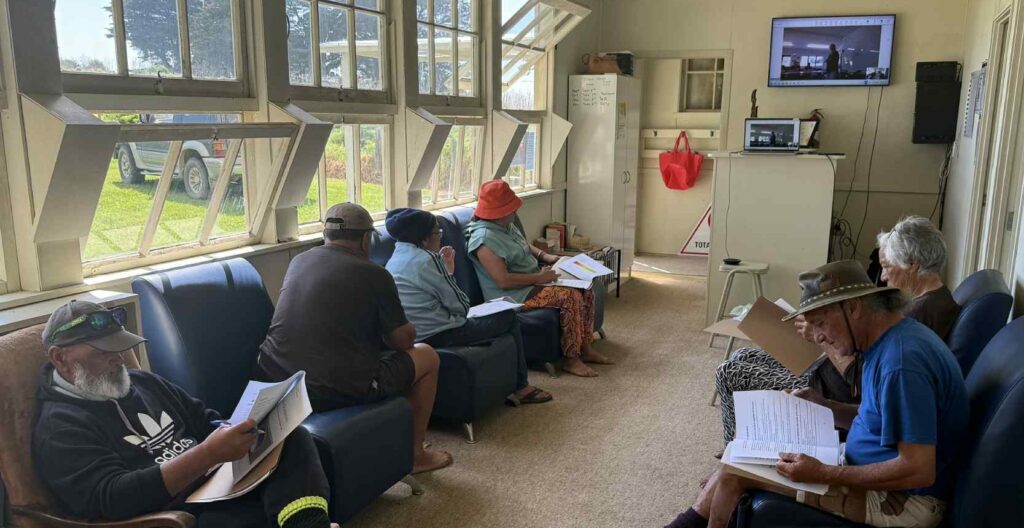
Community Nutritionist Amy Allport, who facilitated the sessions, says tailoring the discussions to whānau was essential. “We shaped each part of the information around what life is like on the island. We had a lively discussion about kai, focusing on meals those in the room enjoyed preparing and eating. We looked at simple ways to make boil-ups healthier and how to plan healthy kai with access to stores being so challenging.”
WBOP PHO Clinical Services Lead Sarah Johnson says the sessions were lively and grounded in whanaungatanga. “There was lots of interaction, strong engagement and some good belly laughs. Co-design made the difference.” She says the energy in the room carried into the following days. Whānau were soon using their exercise bands, restarting their walking group and asking about gym memberships.
What comes next
The project team now plans further wānanga on gout, HPV, asthma and smoking cessation, while keeping support from the first sessions strong. Sarah explains that whānau who need extra help will be linked with the right services. “This may include one-on-one time with dietitians, ongoing nutritional sessions or medication support with our diabetes team.”
Moira notes that the direction continues to come from whānau. “This work shows what is possible when services are designed with communities and not for them.”
What whānau are saying
“We have a big whānau history of diabetes where many have died. I don’t have
diabetes but I’m here to learn so I can share the information with my whānau and mokopuna.”
“Wish this was around 20 years ago.”
“After the food label reading session, I will be taking things out of my pantry and
not letting my mokopuna eat some foods.”